Author: Maitena San Juan
Creutzfeldt-Jakob neurodegenerative disease (CJD) is a prion disorder caused by the misfolded form of the cellular prion protein (PrPC), also known as PrPSc. Its most common variant is the sporadic form (sCJD), which accounts for approximately 90% of the cases of prion disease diagnosed in humans and is of completely unknown cause. The clinical symptoms are diverse, although characterised by rapidly progressive dementia, which makes diagnosis difficult due to similarity to other more common neurodegenerative processes. Diagnosis before death is currently based on imaging tests and the detection of indirect markers of neuronal damage in cerebrospinal fluid (CSF), such as elevated levels of 14-3-3 protein. Recently, the detection of PrPSc in CSF by RT-QuIC has gained relevance due to its high accuracy in the diagnosis of sCJD. However, discrepancies have been observed between 14-3-3 and RT-ICR results.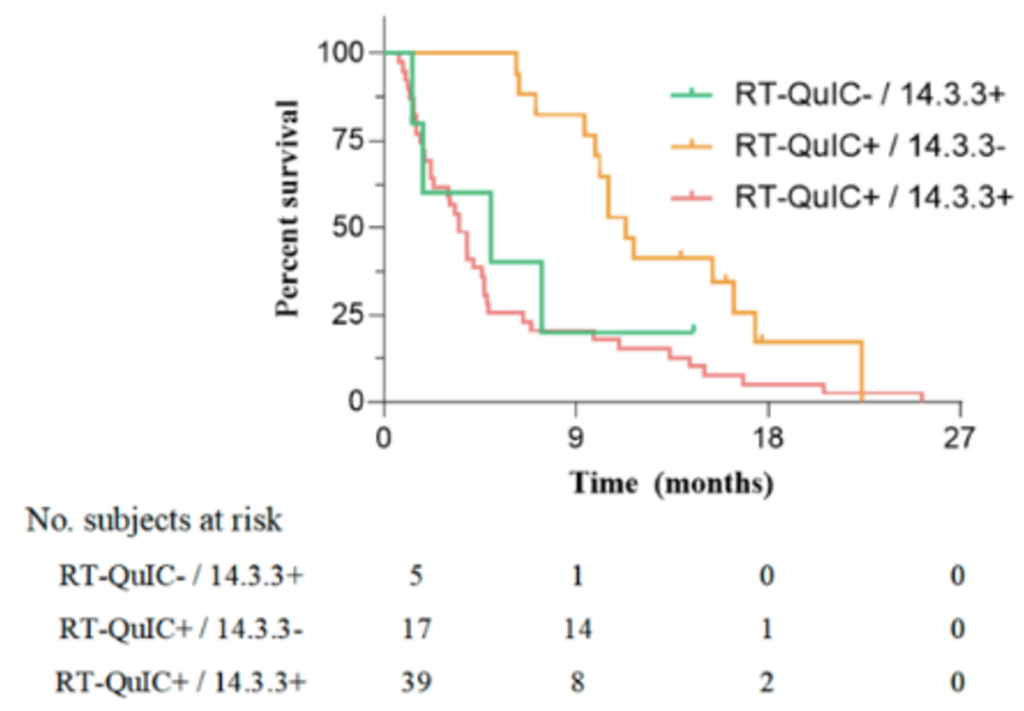
To assess the concordance and usefulness of both techniques, a group of researchers at Hospital Clínic de Barcelona analysed the CSF of 374 patients with suspected sCJD over a four-year period. The results showed that patients positive only for RT-ICRT had slower disease progression and a longer median survival time. In addition, the RT-QuIC technique showed a sensitivity (the ability of a test to correctly detect true positives) of 92.1% and a specificity (the ability of a test to correctly identify true negatives) of 98.9%, while the values for 14-3-3 protein were significantly lower (73% and 62.8%, respectively). Since elevated levels of 14-3-3 are not specific to prion diseases, they are also present in other neuronal events and neurodegenerative disorders.
Figure representing the mean survival of patients according to their CSF biomarker profile: in green, those positive only for 14-3-3 protein; in yellow, those positive only for RT-QuIC; and in red, those positive for both techniques.
This study positions the detection of PrPSc by RT-QuICR as a sensitive and effective tool for pre-death diagnosis of sCJD, linking a positive RT-QuICR result to a slightly slower disease course. However, more research is needed to determine whether the longer disease duration and less neuronal damage in RT-QuICR-positive patients is due to diagnosis at an earlier stage of the disease or to differences in the pathological mechanisms of the patients.
See original article, here.