Author: Eva Fernández-Muñoz
Creutzfeldt-Jakob disease (CJD) is a rare, rapidly progressive neurodegenerative disorder caused by the misfolding of the cellular prion protein (PrPC) in a misfolded form called PrPScwhich accumulates in the brain, causing neuronal damage and spongiform degeneration. The sporadic form (sCJD) is the most common, accounting for approximately 85% of cases, with the remainder due to genetic or iatrogenic causes of the disease. Moreover, it is lethal within months of symptom onset, and its low prevalence, combined with the variability of its clinical presentations, makes early diagnosis very difficult.
A recent study conducted in Austria between 2013 and 2020, which combined data from the Austrian Reference Centre for Prion Diseases and national health insurance registries, has identified that mood disturbances, such as anxiety or depression, could be an early sign of spontaneous disease. In the study, data from 129 patients with a confirmed diagnosis of sCJD after their death were analysed and compared with 1,350 controls (without a diagnosis of the disease). The researchers found that patients were more likely to have been prescribed antidepressants, such as selective serotonin reuptake inhibitors (SSRIs), in the year prior to diagnosis. This increase began up to three years before the onset of typical neurological symptoms.
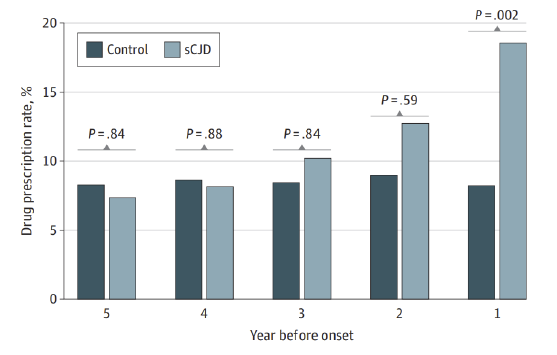 Figure of results showing prescription rates of selective serotonin reuptake inhibitors (SSRIs) in patients with sporadic Creutzfeldt-Jakob disease (sCJD) (light blue) and controls (green) in the 5 years prior to disease onset (or before the index date in control individuals).
Figure of results showing prescription rates of selective serotonin reuptake inhibitors (SSRIs) in patients with sporadic Creutzfeldt-Jakob disease (sCJD) (light blue) and controls (green) in the 5 years prior to disease onset (or before the index date in control individuals).
Mood changes, such as depression or anxiety, may be part of the prodromal phase of SCJD, a disease that progresses rapidly and lacks definitive diagnostic tools. premortem. Although neurological symptoms include rapid dementia, ataxia and myoclonus, the early stages are often missed or confused with other conditions. This finding on mood swings stands out as a possible early indicator and could help advance research into other neurodegenerative diseases. However, limitations of the study include: lack of detailed clinical information in the insurance data, bias due to regional differences in medical care, and exclusion of medications administered in hospitalisations or purchased over the counter.
See the original study (in English).